Am I the only one experiencing this phenomenon or are more and more people we know being diagnosed with bipolar disorder (BD)?
Bipolar disorder involves periods of elevated or irritable mood (mania),
alternating with periods of depression. The “mood swings” between
mania and depression can be very abrupt. (National Center for
Biotechnology Information, U.S. National Library of Medicine)
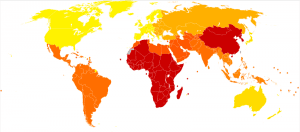
In 2002, the World Health Organization produced the Bipolar disorder world map depicted below with the greatest impact of BD occurring in the red regions (as measured by the cumulative number of years lost due to ill health, disability or early death).
Bipolar disorder world map – DALY – WHO2002.svg
Disability-adjusted life year for bipolar disorder per 100,000 inhabitants in 2002.
less than 180
(yellow) 180–186
186–190
(lt. gold) 190–195
(gold) 195–200
200–205
205–210
(orange) 210–215
215–220
220–225
225–230
(red) 230–235
Whether this rising awareness is global fact or fiction, an increased prevalence of BD diagnosis is emerging in my colleagues and clients. Some might argue my greater awareness is simply due to a greater willingness on the part of those with BD to shun the stigmatism of mental illness and talk openly about their experience. Certainly, there is truth in this statement. For someone who espouses self-compassion as a profoundly transformative healing behavior, I am delighted. It means we are denting the “conspiracy of silence” pattern that predominated my youth and adulthood by offering ourselves loving kindness and eliminating self-judgment.
However, along with such good news travels some unanswered questions. In my research on this topic, the general (though understated) consensus appears to be that BD is both difficult to diagnose and to treat. Likely this correlates with the fact that there are no biological/laboratory tests or x-rays for BD. The US National Library of Medicine states “the exact cause is unknown, but it occurs more often in relatives of people with bipolar disorder. . . Treatment strategies for children and the elderly have not been well-studied, and have not been clearly defined.”
Wikipedia counters with “the causes of bipolar disorder likely vary between individuals . . . [Hereditary] results are not consistent and often not replicated . . . [and] evidence suggests that environmental factors play a significant role in the development and course of bipolar disorder.”
Foremost in my mind, is — if this illness is so poorly understood relative to cause, treatment and prognosis, why is the standard solution drug therapy? In particular, such potent narcotics as mood-stabilizers, anti-depressants, anti-psychotics and addictive anti-anxiety medications?
I am reminded of the medical treatment many women in the late 60s and early 70s received for their “dissatisfaction with life” and “emotional depression” — valium. When I was 16, I stayed with one of these women while she was medicated. She was barely able to walk or talk while awake and slept 20 of the 24 hours in a day. I had to wonder which was worse — the treatment or the disease? The medical profession had its knuckles publically rapped for that faux pas.
Does this propensity for our medical model of illness to “deal drugs” to an already over-medicated society still prevail? This is not to say that many drug therapies aren’t necessary and welcomed treatments but they are not the only healing tools available, and they typically are short-term interventions not long-term cures. More importantly, when there is no identifiable biological connection, then what is being treated? Just as when I was 16, are medical professionals administering drugs because it makes it easier for the rest of society to deal with mental illness?
The data suggests environmental stressors (recent life events, interpersonal relationships, traumatic/abusive experiences in childhood, post-traumatic stress disorder) significantly increase one’s potential for experiencing BD. These stressors are on the increase globally and will not be going away in the near future. They are typically treated and relieved with psychotherapy, which begs the question – Why isn’t psychotherapy a standard treatment practice for BD rather than merely a support methodology, as appears in most of the literature?
Why not use meditation, yoga, naturopathy or other holistic treatment approaches as well? Countless research studies show the many benefits of these so called “new age” methodologies in relation to handling a variety of stressors. Why aren’t these less invasive strategies prescribed first and pharmacology provided as a last resort? Does it feel like the traditional healthcare arena still has an iron-clad grip on how we receive treatment?